This month, we are delighted to publish another fantastic study from the COVIDSurg and GlobalSurg collaboratives who were recently awarded a Guinness World Record for work previously published in the journal. This new paper comes from 15,025 global authors based in over 1600 hospitals and reports data for 96,454 patients. The topic this time is pre-operative isolation, which was introduced as a precaution despite limited evidence on its benefits and harms. It aims to keep systems clean and patients safe, but is it risk free? They found that, following correction for various measured confounders, it was associated with a small but clinically important increase in postoperative pulmonary complications (Fig 1). In the associated editorial, Charlesworth and Grossman set out how this new information may help us move towards ‘COVID-19 secure’ elective surgery. If indeed pre-operative isolation is not without risk, then hospitals need to focus on how this may be tackled as well as other ways in which nosocomial transmission can be prevented.

One such area where there remains room for improvement is incorporating what we now know about ‘aerosol-generating procedures’ into policy documents, guidelines and local procedures. This new study from Wilson et al. yet again shows that therapies such as high flow nasal oxygen and continuous positive airway pressure generate less aerosol as comparted with breathing, talking, exercising, shouting or coughing. Such therapies should not therefore be delayed in patients with COVID-19 and we should instead focus on ‘aerosol-generating patients’, not procedures. Also featuring this month is a new Association of Anaesthetists guideline for regional analgesia for lower leg trauma and the risk of acute compartment syndrome. This guideline generated a lot of debate on social media and the associated podcast provides some useful context. Perhaps one of the main talking points was recommendation six, which stated that neither the surgeon nor the anaesthetist has the right to veto a treatment recommended by the other. The associated editorial from Bogod and McCombe expands upon the associated controversies including aspects of patient ownership and autonomy. They also discuss the reasons why the British Orthopaedic Association were unable to endorse the final document. The editorial from Keating and Duckworth focusses on clinical aspects of the guideline with particular emphasis on the need for more monitoring in acute compartment syndrome. Such monitoring has been available now for over three decades and perhaps enables patients to receive appropriate analgesia appropriate to the circumstances.
For patients who have suffered traumatic injuries, reducing time from injury to definitive care is perceived to be associated with improved health outcomes. This new retrospective analysis of linked registry data from Lyons et al. aimed to evaluate the effect of the introduction of the Emergency Medical Retrieval and Transfer Service (EMRTS) on 30-day mortality in patients who had suffered blunt traumatic injuries (Fig. 2). After adjustment for differences in case-mix, they found a 37% reduction in the adjusted OR for 30-day mortality in patients with blunt traumatic injuries who were treated by EMRTS compared with standard pre-hospital care pathways. Hurst and Lendrum remind us of the reasons why this was not a good comparison of ground vs. helicopter emergency medical systems, but there remain some important clinical messages. For example, there is a need to include all trauma patients in national registries and establish why injured patients die in the early post-injury phase.

Postoperative sleep disturbance is perhaps more common than we think with significant consequences for patients. Earplugs and eye masks are low-cost interventions that may help, yet this is an area which has received little attention in the peri-operative literature. Leong et al. report their randomised controlled trial of effect of the use of earplugs and eye masks on the quality of sleep after major abdominal surgery. They did not find that the use of earplugs and eye masks as sleep aids on postoperative days 1–3 improved the sleep quality of patients after major abdominal surgery, nor did it affect patient satisfaction, reduce the frequency of nursing care required or reduce the incidence of delirium. We look forward to receiving more original articles in this area and there is much to be done.
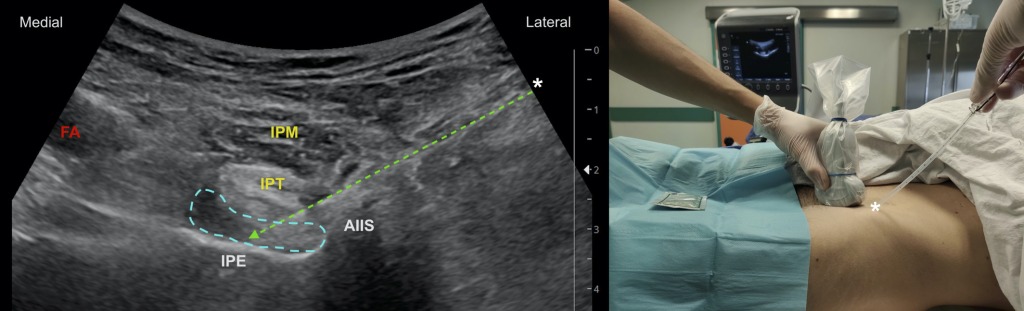
Severe pain after total hip arthroplasty can have major negative effects on recovery and mobilisation in the postoperative period. Pascarella et al. report their randomised observer-masked controlled trial of the impact of the pericapsular nerve group (PENG) block on postoperative analgesia and functional recovery following total hip arthroplasty (Fig. 3). They found that the PENG block improved postoperative analgesia following total hip replacement, and decreased pain scores and opioid consumption during the first 48 h after surgery. Time to now consider it as a valid analgesia option for fast-track hip surgery protocols? Finally, Finnerty et al. report their randomised trial of bilateral erector spinae plane block vs. no block for thoracolumbar decompressive spinal surgery. They found that the addition of intra-operative erector spinae block to multimodal analgesia improved recovery and reduced pain up to 24 h after thoracolumbar decompressive spinal surgery. Perhaps another indication for a block that has exploded in popularity despite being discovered and reported for the first time only recently.
Elsewhere we have: a review of oxytocin at birth and beyond; an observational study of temporomandibular joint dysfunction following the use of a supraglottic airway device during general anaesthesia; and a randomised controlled trial of the effect of saline versus air for cuff inflation on the incidence of high intra-cuff pressure in paediatric MicroCuff® tracheal tubes.
Make sure you check out our top 10 papers of 2020 which we announced only last week at an excellent Annual Congress virtual conference! Congratulations to El-Boghdadly and team for winning paper of the year which was all about risks to healthcare workers following tracheal intubation of patients with COVID‐19!
Mike Charlesworth and Andrew Klein




Thanks a lot for sharing this amazing post, monthly patient safety
LikeLike