Seven years ago, the results from the Fourth National Audit Project (NAP4)were published. A key conclusion was that awake fibreoptic intubation (AFOI) may have prevented several reported cases of airway-related morbidity and mortality, especially where difficulty was anticipated. The resultant recommendation was that all anaesthetic departments should provide a service where the skills and equipment are available to deliver AFOI when indicated. Though not explicitly stated, AFOI was seen thereafter, by many, as the ‘gold standard’ for difficult airway management.
Three years ago, Ahmad and Bailey suggested AFOI was becoming obsolete due to the emergence of other devices, such as the videolaryngoscope. Today, Alhomary et al. report the first systematic review and meta-analysis of videolaryngoscopy vs. fibreoptic bronchoscopy for awake tracheal intubation (ATI). They conclude intubation with videolaryngoscopy is quicker and has a similar success rate and safety profile as compared with AFOI. Their paper currently holds an Altmetric score of 226, which makes it the 8thmost shared and discussed paper from the journal, ever! In their editorial, Wilson and Smith discuss the clinical practice and study of ATI and how it presents significant problems to systematic reviewers. Their concluding argument is ATI with videolaryngoscopy should be a ‘core’ technique for all and a primary technique for novice anaesthetists. Will practice necessarily change in the future? The debate has been fascinating thus far and the arguments for and against will no doubt continue. A popular opinion seems to be that the real ‘skill’ is the technique of airway topicalisation, and Kariem El-Boghdadly has been kind enough to provide us with his recipe (Figure 1).
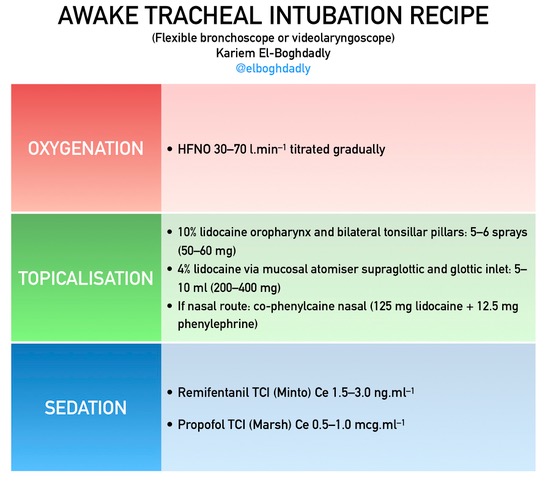
Figure 1 A proposed recipe for oxygenation, topicalisation and sedation for ATI as provided by @elboghdadly.
Is there a gold standard for peri-operative neuromuscular blockade? Ask a surgeon and they may suggest it should be the provision of optimal operating conditions.This study from South Korea suggests deep neuromuscular blockade is indeed associated with better surgical conditions as compared with moderate blockade in patients undergoing laparoscopic surgery. Ask an Intensivist, however, and they might suggest neuromuscular blockade should be undertaken in a manner that reduces the incidence of postoperative pulmonary complications. This multifaceted quality improvement project from Massachusetts General Hospital was able to do just that through optimising the documentation of TOF monitoring and the dosing of neostigmine (Figure 1).

Figure 2 Neuromuscular blocking agent dosing guide used at Massachusetts General Hospital as a cognitive aid in the quality improvement initiative. TOF, train‐of‐four.
In fact, their suggestion, that we should avoid the use of neostigmine when the degree of neuromuscular blockade has not been determined, may be supported by this next paper. Kent et al. present their results from a randomised controlled trial of neostigmine and glycopyrrolate given to healthy volunteers in the absence of neuromuscular blockade as compared with placebo. They conclude those given neostigmine and glycopyrrolate developed clinically significant muscle weakness which shared certain characteristics with a phase-1 depolarising block and may not be apparent with TOF monitoring. In their editorial, Naguib and Kopman argue these results have little or no clinical significance and anxiety around neostigmine-induced weakness is misplaced and unnecessary. Perhaps access to quantitative neuromuscular monitoring should be the real gold standard with regards the management of peri-operative neuromuscular blockade? If indeed it is, we still have a long way to go!
How best to manage, all at once, peri-operative neuromuscular blockade, depth of anaesthesia, coagulation, haemodynamics, mechanical ventilation and analgesia? In their editorial, Fawcett and Jones argue the technology exists to manage all these aspects of peri-operative care and more, but the anaesthetist should remain firmly at the controls. The general message seems to be that patients should be treated according to their individual needs rather than fixed formulas or algorithms, and practice does indeed seem to have evolved beyond the formulaic approach of the past. Does your hospital undertake surgery where blood loss is a recognised complication? If so, these new guidelines on the use of cell salvage for peri-operative blood conservation are essential reading. Again, this paper has already attracted much attention on social media and currently holds an Altmetric score of 113! Perhaps the most striking recommendation is that cell salvage should be universally available 24 hours a day in all hospitals performing major surgery. There is something here for everyone and we wholeheartedly recommend all members inspect these guidelines and discover how their future practice could be affected.
Many would agree the gold standard for generating clinical evidence is a randomised controlled trial, systematic review or meta-analysis. What if the aim is to prove a new, cost-effective intervention is no worse than (or non-inferior to) the current standard of care? So-called non-inferiority studies are increasingly common, yet their design, reporting, and interpretation can be extremely challenging. In this month’s Statistically Speaking, Charlesworth and Choi discuss non-inferiority studies with reference to a recent study from Nakanishi et al. Whether or not such studies should be seen as an inferior form of research methodology perhaps remains debatable, but the study by Nakanishi et al. demonstrates their value as an innovative way in which questions can be asked that cannot be answered by other means.
Point of care viscoelastic tests of coagulation such as ROTEM® are arguably becoming the gold standard for making transfusion decisions in the context of acute haemorrhage. This new study suggests a strong correlation between clot firmness at 5 (A5) and 10 (A10) minutes with maximum clot firmness (MCF). For coagulopathic trauma victims, do we really need to wait for the MCF or can we make early transfusion decisions using A5? Finally, what is the gold standard for critically injured burn patients? In the UK, they should be admitted to specialist burn units, and this new observational study finds that, on the whole, this seems to be the case. Furthermore, a generic risk prediction model outperforms two specialist models in such patients.
Elsewhere this month there is a retrospective study of pre‐operative anaemia, intra‐operative hepcidin concentration and acute kidney injury after cardiac surgery; a comparison of peripheral nerve blockade characteristics between non‐diabetic patients and patients suffering from diabetic neuropathy; a study of real‐time injection pressure monitoring system to discriminate between perineural and intraneural injection of the sciatic nerve in fresh cadavers; and the description of a new analgesic index using nasal photoplethysmography.
Over in Anaesthesia Cases there is an excellent case report of eFONA along with a discussion of how new guidelines and practices seem to be changing the skillset and role of the anaesthetist. Later this month, the Association of Anaesthetists will be holding their Annual Congress meeting in Dublin. The Anaesthesiajournal session takes place on Friday morning and first up will be Professor Mike Irwin discussing the advantages and disadvantages of remifentanil. This year, Matt Wiles hosts the ‘Anaesthesia article of the year’ and we look forward to finding out who made this year’s Top 10! Other highlights will include Professor Tim Cook discussing ‘Videolaryngoscopes for all?’ and we will, once again, be running our popular ‘How to publish a paper’ workshop. Finally, it’s all change at the association, and we are delighted to see our new design online for September. Printed journals should be landing from the 3rdof September onwards and you can read all about the new brand of the Association of Anaesthetists in your new-look Anaesthesia News.

See you in Dublin!
Mike Charlesworth Andrew Klein
Trainee Fellow Editor-in-Chief




You must be logged in to post a comment.