There has been concern for some time in some areas of the UK that critical care admission is rationed according to age. This new retrospective observational study from Pugh et al., which was conceived and conducted before the outbreak of COVID-19, aimed to investigate trends in patient characteristics for adult critical care admissions in Wales between 2008-2017. They analysed 85,629 cases with the oldest cohort (≥ 80 years) accounting for 15% of critical care admissions. The proportions in each age bracket did not change over the study period. However, in contrast to several recent reports, they identified a significant decline in admissions of older patients (aged ≥ 65 years) relative to the national population, of those with comorbidity and those with a medical diagnosis (Fig. 1).

Has critical care capacity failed to keep pace with the needs of an ageing population? Lone and Suntharalingam make a case for the need to learn, adapt and ensure equity and appropriate best care for our growing cohorts of those aged > 65 years and new octogenarians. That said, the priority for many older critically unwell adults is not always survival at all costs. What will anaesthesia and peri-operative medicine look like to us when many of the current workforce are classed as an older adult in ~25 years? Fawcett and Klein discuss the implications for genomics, AI, service delivery, peri-operative medicine, green anaesthesia and radiology. The only certainty seems to be that our skills will continue to be in demand and there will inevitably be significant workforce shortages.
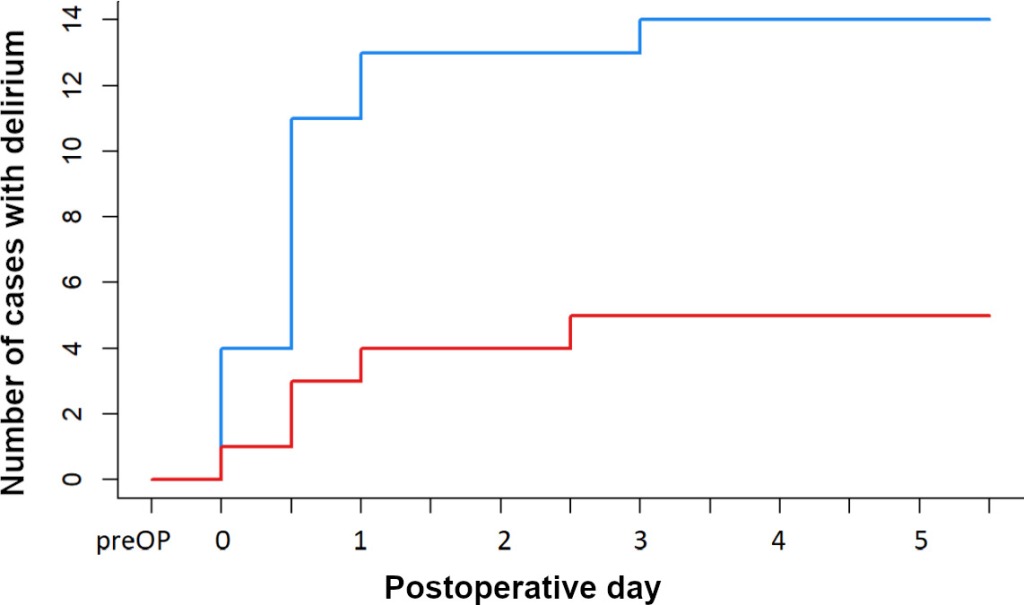
Dexmedetomidine is now used widely for several indications in peri-operative practice and critical care medicine. This new randomised controlled trial from van Norden et al. is the first to investigate the effect of peri-operative administration of dexmedetomidine on the incidence of postoperative delirium in major cardiac and non-cardiac surgical patients aged > 60 years. They found that found a significant reduction in postoperative delirium to 18% from 44% when dexmedetomidine was administered as compared with placebo (Fig. 2). In the accompanying editorial from Chuan and Sanders, the biological plausibility of this finding is assessed, and dexmedetomidine might not be the much sought-after magic bullet for the prevention of postoperative.
This new science letter from Shah et al. reports results from a retrospective cohort study of general ICU survivors in two large health regions in the UK aiming to benchmark how many patients had anaemia-specific treatment (excluding blood transfusion) initiated before hospital discharge. The key findings were: a high prevalence of anaemia at ICU discharge and subsequently hospital discharge; little active management of anaemia during this important time period; and Hb of < 100 g.l-1 was associated with prolonged hospitalisation following ICU discharge. Also in this month’s issue, van der Laan et al. report their retrospective analysis of anaemia among intensive care unit survivors and its association with days alive and at home. They found that among ICU survivors, anaemia was highly prevalent and persistent in most patients at hospital discharge. Haemoglobin concentration < 100 g.l-1 at ICU discharge was experienced by 2886 (45.4%) of ICU survivors and independently associated with five fewer days alive and at home to day 90. This association remained significant when accounting for confounders including ICU length of stay, illness severity and red blood cell transfusion, and was attributable predominantly to fewer days at home among anaemic ICU survivors. In addition, ICU discharge anaemia was also an independent predictor of ICU and hospital re-admission (Fig. 3). In the accompanying editorial, Agarwal and Karkouti discuss both studies and remind us that the findings from each might at best be hypothesis generating only. They remind us of the vast amount of work still to be done in what is becoming and increasingly important area of clinical practice.

We are delighted to publish a Special Article from Takla et al. in this month’s issue, which raises some difficult ethical and legal issues around the use of general anaesthesia in end-of-life care. They remind us that our speciality already has a self-declared mission to extend the role of anaesthetists beyond the operating theatre in its strategy of championing ‘peri-operative medicine’. They argue that their redefinition of the scope and reach of general anaesthesia through end-of-life care, radical though it is, would be entirely in line with that philosophy, recognising that anaesthetists have skills that can help alleviate suffering for the dying patient. Their main findings were that peri-operative lidocaine infusions of extended duration can be delivered safely and effectively in patients undergoing breast cancer surgery, and that a definitive, multicentre trial employing these design features is feasible.
One of our most popular podcasts episodes was about the use of intravenous lidocaine in peri-operative practice released November 2020. This new pilot multicentre randomised controlled trial of lidocaine infusion in women undergoing breast cancer surgery from Toner et al. enrolled 150 patients and looked at safety, effectiveness and the feasibility of a larger trial. Daliya et al. report their retrospective observational study of Opioid prescription at postoperative discharge. They were able to isolate a number of recognised risk-factors in the prescribing habits of clinicians at discharge that could contribute to a large unused pool of opioids in the community. In the accompanying editorial, Albrecht and Brummett remind us that if you cannot measure it, you cannot improve it. They argue that improvement can be made through: proper adherence to education and guidelines; by embracing simple measures such as prescription of non-opioid analgesics at regular intervals; specification on the duration of the course of immediate-release opioid tablets; avoidance of long-acting opioid formulations and compound analgesic preparations; and advice on deprescribing.
Elsewhere this month we have: a systematic review of suicide in anaesthetists; a systematic review of simulation-based team training in airway management; new Association of Anaesthetists fire safety and evacuation guidelines; and a time-sensitivity analysis of the prognostic utility of vasopressor dose in septic shock.
Finally, make sure you do not miss our next live broadcast with our Associate Editor Dr Tanya Selak chairing which is all about a new paper on the safety of day-case paediatric tonsillectomy in England from the Getting It Right First Time programme. You can tune in by coming to @Anaes_Journal (or following this link) at 1200 BST on Friday 17th September!
See you then!
Mike Charlesworth and Andrew Klein



You must be logged in to post a comment.