We are delighted to announce that our 2024 special supplement will focus on sustainable healthcare and the role of the anaesthetist. This month’s issue shows how important this theme is also in 2023. First, Waspe and Orr review regulatory guidelines for environmental risk assessment of propofol in wastewater. They outline the two phases of an environmental risk assessment for medicinal products and remind us that other drugs such as: erythromycin; clarithromycin; ibuprofen; diclofenac; ethinylestrodiol; metformin; and propranolol have the highest ecotoxicological risk to the surface water environment. In the associated editorial, White, Fang and Shelton outline the propofol life cycle (Fig. 1). Their interpretation is that ‘worst-case’ propofol wastewater exposure estimates fall far below the threshold at which aquatic species sustain adverse effects. They call on all anaesthetists to continuously make incremental progress in understanding and lowering our professional environmental impact.

Medicinal nitrous oxide use has well described consequences for the environment and this new editorial from Lucan et al. accompanies a paper from 2022 by Pinder et al. They remind us that there is no simple switch from nitrous oxide for labour analgesia and this makes the balance between patient choice and environmental concern a delicate one. They call for more widespread implantation of ‘cracking devices’ in delivery units across the UK. Getting it right first time is key to reducing out environmental impact, and this new editorial from Coldwell and Craig outlines how this might be done by better deploying anaesthetic skills and workforce. One interesting point relates to who trainees should anaesthetise with distant supervision and how this has changed over time. There remain many questions and concerns about the anaesthetic workforce, and we will no doubt see this becoming an important issue over the coming years.
Tranexamic acid is a useful adjunct to reduce peri-operative bleeding and the need for blood transfusion. This new population-based study from Taiwan looked at 226,719 total knee replacements during 2010–2019. They found that tranexamic acid treatment was associated with a 50% decrease in red blood cell transfusion rates, with no increased risk of all vascular outcomes or in-hospital mortality. However, they did identify an association between TXA use and an increased risk of renal injury (Fig. 2). In the associated editorial, Bailey summarises the evidence for tranexamic acid in total knee arthroplasty. He argues it is effective, affordable and safe, and that its use should be enshrined in routine practice.

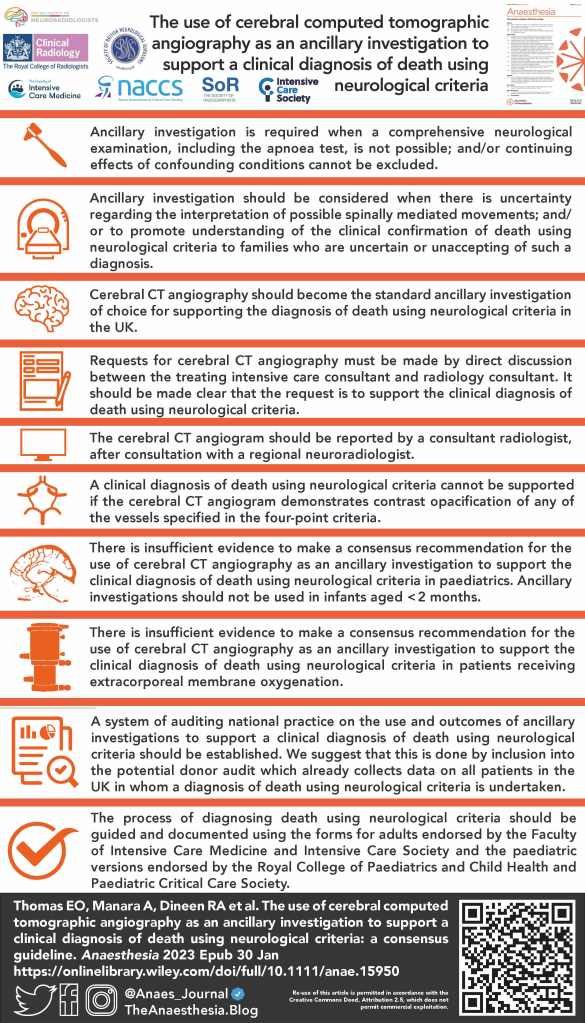
This new multicentre retrospective cohort study from Suleiman et al. tackles an old question – which reversal agent is best? They included 83,250 patients from 2016–2021 and found no association between the choice of the primary reversal drug and postoperative respiratory complications or advanced healthcare utilisation. Equivalence and non-inferiority were also established between sugammadex and neostigmine. Another therapy under question is pre-operative intravenous iron before major abdominal surgery for iron deficiency anaemia. This secondary analysis of the PREVENTT trial found no beneficial effect of the use of intravenous iron compared with placebo, regardless of the metrics to diagnose iron deficiency, on postoperative complications or length of hospital stay. There are several other clinical implications of this research that are discussed in depth in the associated free podcast. Another important paper is a new multidisciplinary consensus statement on the use of cerebral computed tomographic angiography as an ancillary investigation to support a clinical diagnosis of death using neurological criteria. Cerebral CT angiography has been shown to have 100% specificity in these circumstances and is an investigation available in all acute hospitals in the UK. There are 10 recommendations which are essential reading for all intensivists, radiologists, radiographers and neurosurgeons.
Elsewhere we have: a randomised controlled trial of intravenous dexmedetomidine added to dexamethasone for arthroscopic rotator cuff repair and duration of interscalene block; a review of cognitive aids in the management of clinical emergencies; a review of postoperative systemic inflammatory dysregulation and corticosteroids; and a systematic review of dexmedetomidine for adult cardiac surgery.
This month, we have two ‘Reviewer Recommendations’ papers which tackle how to perform and write a trial sequential analysis and how to write a Science Letter for Anaesthesia. Our aim is that these articles not only help those who wish to submit their work to the journal, but they are of wider use to all who wish to learn more about research methods and how papers are published.
Finally, we are advertising for new Editors and a LMIC-based Editorial Fellow. We hope you will consider joining our team.



Mike Charlesworth and Andrew Klein